
CASE STUDY: A 59-year-old FIFO mine site truck driver smoked 15 cigarettes per day from adolescence until five years ago. Two years ago, she developed asthma following a viral respiratory infection. Subsequent symptoms of cough, wheeze and tightness have been relieved by salbutamol MDI, used up to six times a day.
Her symptoms are not well controlled and so preventive therapy – fluticasone: salmeterol fixed dose combination – two puffs twice daily is prescribed.
Six weeks later she fell asleep driving a truck on a night shift. She has some difficulty sleeping during daytime when on night shift, denies snoring, but wakes frequently mostly with cough and takes Ventolin (2 -10 puffs of per day). She reports increasing difficulty walking upstairs at work due to shortness of breath. She takes the Seretide but misses “the occasional dose”. This time COPD is diagnosed (by a different doctor) and a long acting anticholinergic inhaler prescribed.
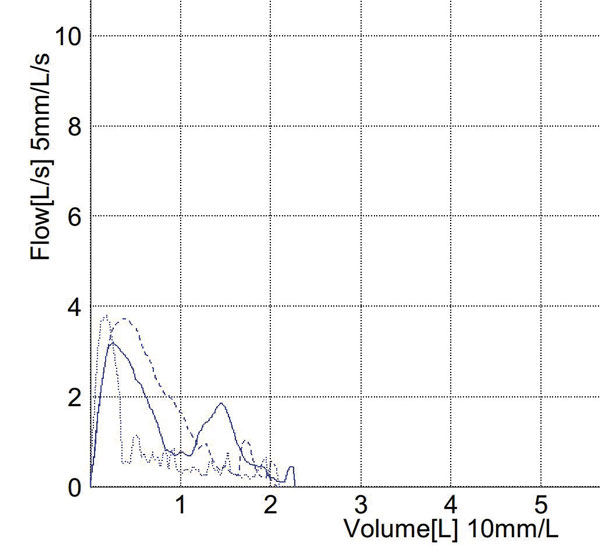
One month later she returns with cough and wheeze and was observed to use her inhaler several times, apparently with limited effect. On examination, she had bilateral inspiratory and expiratory wheeze and prolonged expiratory phase. Spirometry has deteriorated.
She demonstrates poor MDI technique with aerosol escaping from her mouth on actuation of the inhaler; inspiratory timing is poor and she appears to have nasal breathing. She stated that she uses Ventolin at about the same frequency as at the first visit, occasionally using Seretide in place of Ventolin for relief, claiming it does not work as well. She is reluctant to take Seretide because it “contains a steroid” and she had recently gained weight. She refused to use the LAMA because she disagreed with the diagnosis of “emphysema”. When asked if there were days when she did not use Seretide, she admitted forgetting to use it most days.

Key issues:
Does she have asthma or COPD? Smoking 27 pack years is sufficient to cause COPD in a susceptible individual. However, symptoms in the past two years, including response to salbutamol, are consistent with asthma. Assuming correctly performed spirometry, asthma has been confirmed by objective measurement even though COPD may also be present.
Communicating the diagnosis to the patient consistently and effectively is an important prerequisite for patient engagement in asthma management, and outcome. She would benefit from formal asthma (and COPD) education partly to dispel misinformation, like the systemic effects of low-dose inhaled steroids.
Her usage of inhaled steroids has been insufficient to control her asthma. She may have given the impression she was using her inhalers regularly, either because the appropriate question was not asked, or it was the answer the patient thought the doctor wanted.
She has nocturnal asthma causing significant sleep disturbance, morning tiredness and daytime sleepiness (or the reverse with nightshift). Frequency of nocturnal asthma symptoms is a measure of poor control increasing the risk of severe exacerbation, time off work and mortality.
Outcome and discussion
Following education, including MDI technique and supervised trial of inhaled steroid/LABA twice daily, regular assessment and reinforcement, she reported progressive improvement of asthma symptoms sleep quality and reduced salbutamol consumption. Spirometry improved progressively allowing back-titration of ICS dose. LAMA was withdrawn.
Physicians generally overestimate their patients’ inhaler adherence rates and, even when their estimates are conservative, they are usually wrong. Non-adherence may be intentional (e.g. patient rejects diagnosis), or unintentional (e.g. poor technique). The latter is often linked to psychosocial, demographic and comorbidity factors. Both forms may be amenable to education.
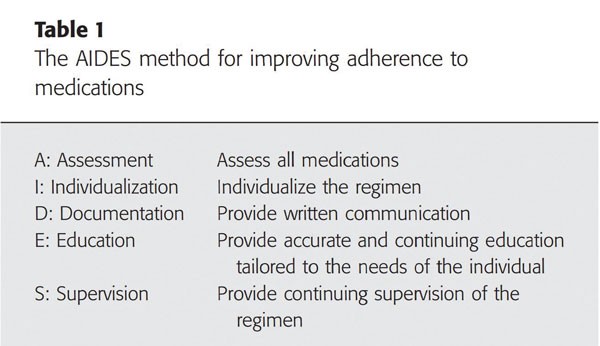
Published estimates of adherence to inhaler therapy in asthma range from 30-70%, and is determined by many factors, including health beliefs, understanding of and attitude towards asthma, effectiveness of therapy and psychosocial factors. The professional relationship with the patient is an important factor in determining outcome, including adherence to treatment. That relationship is best viewed as a partnership (therapeutic alliance), in which there is asymmetric knowledge.
Patient communication is our responsibility. It starts with asking the right questions such as: ‘Many patients don’t take their inhalers all the time. In the past month or two, how many days per week would you have taken your preventer inhaler?’ These are better than questions such as: ‘Do you take your asthma inhalers?’
If stated adherence is low, then non-judgementally ask why. For example: ‘Do you have any concerns about the effectiveness of the medication, or any side effects?’, and, ‘Let’s have a look at how you use your inhaler’.
Adherence matters because those adhering to prescribed ICS/LABA inhalers have few symptoms, longer time to exacerbation, lower exacerbation rates, fewer admissions to hospital, reduced mortality and overall lower healthcare costs.
References available on request.
Questions? Contact the editor.
Author competing interests: nil relevant disclosures.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

