
ED: As the incidence of diabetes grows, so do the side effects. Retinopathy is one and the changes in recent years, particularly pharmacotherapy, mean a lot to patients.
Diabetic retinal disease could become a major public health challenge. About 1 in 20 Australians are now diagnosed with diabetes, and Australia’s diabetic population is expected to reach 3 million by 2025. This will lead to a steep rise in diabetic eye disease, the leading cause of vision loss in the working-age population.
Significance increases when you consider one third of patients with diabetes have diabetic retinopathy, and in one third of these cases vision is threatened, requiring prompt treatment.
Visual impairment in diabetes results from microvascular damage to retinal capillaries via distinct pathophysiological pathways:
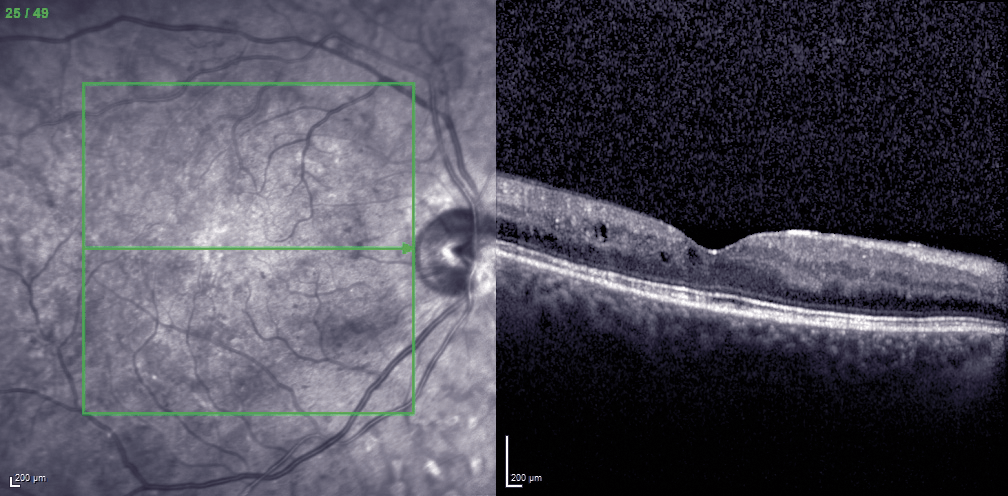
- Diabetic macular oedema (DMO): leakage from capillaries within the central macular area of the retina causes retinal thickening and loss of function. Vascular endothelial growth factor (VEGF) has been shown to increase vascular permeability in vivo and is an important mediato VEGF levels are increased in the retina and vitreous of eyes with diabetic retinopathy and DMO, and inhibition of VEGF therefore targets the underlying pathogenesis.
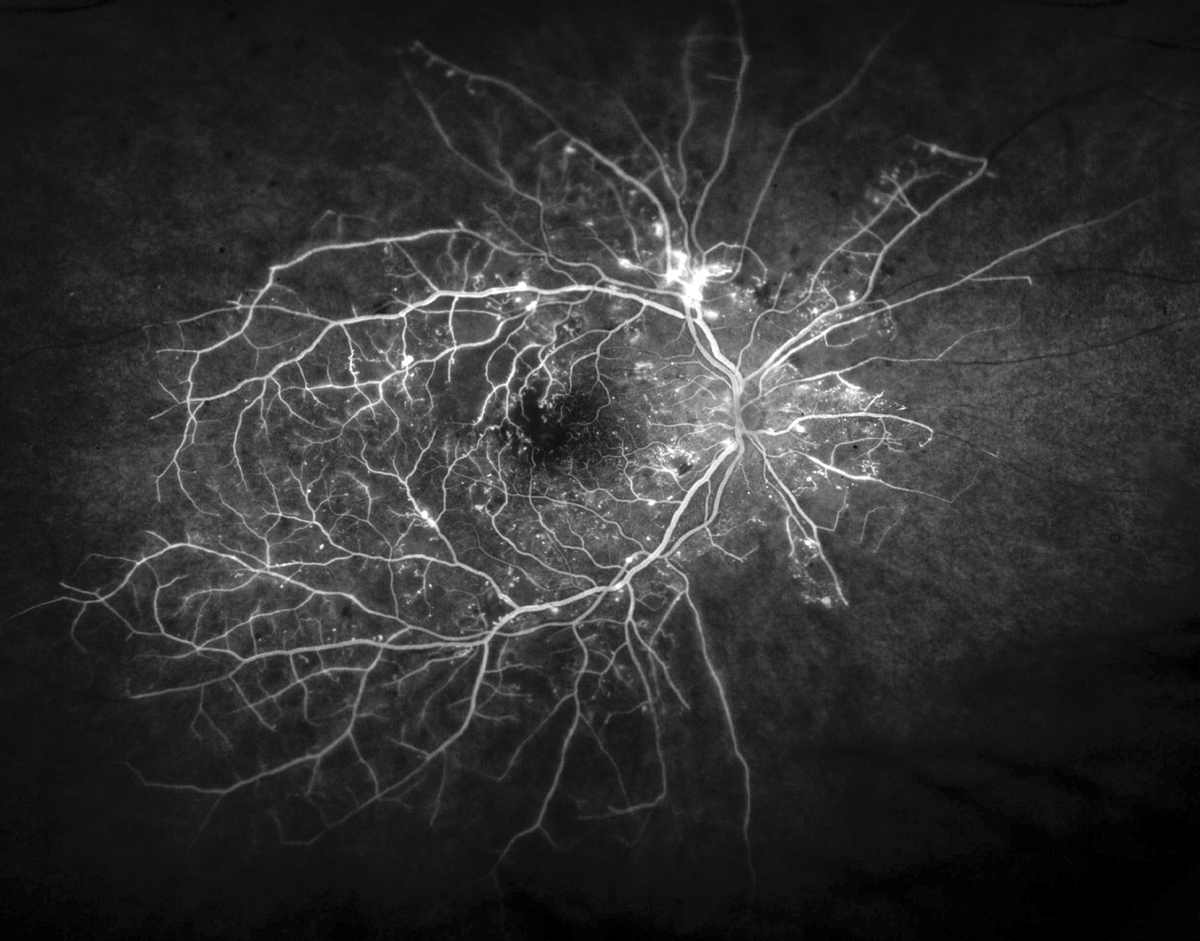
- Proliferative diabetic retinopathy (PDR): blockage of retinal capillaries causes ischaemia, stimulating new blood vessel growth with resulting haemorrhage and retinal tractio
Screening for diabetic retinopathy
Appropriate treatment of sight-threatening retinopathy requires identification of patients at risk. Fewer than half of all Australians with diabetes and only one in five of Indigenous Australians receive the recommended eye examinations. The two primary risk factors predicting retinopathy severity are duration of diabetes and poor glycaemic control. Secondary factors include hypertension, elevated plasma lipids, pregnancy and microalbuminuria.
How often? Current NHMRC guidelines recommend an eye examination every two years for non-Indigenous Australians with diabetes, and annual examinations for Indigenous people with diabetes and patients with another risk factor. Optometrists, ophthalmologists or suitably trained GPs can perform screening. Automated retinal image analysis using algorithms capable of detecting diabetic retinopathy lesions in fundus photographs, may in future lessen the clinical screening burden, though they have not been widely adopted due to inadequate sensitivity and specificity.

Management of diabetic retinopathy
Almost all cases of severe visual loss due to diabetic retinopathy can be prevented. Optimal glycaemic control, and management of hypertension and plasma lipids, reduce the risk of retinopathy progression.
Laser photocoagulation: In PDR cases, the landmark Diabetic Retinopathy Study showed that photocoagulation reduced the risk of serious visual loss by more than half, and this remains the most economical and efficient treatment for proliferative disease. Recent clinical trials have shown anti-VEGF injections to be non-inferior to photocoagulation, but the requirement for ongoing treatment is expensive and onerous.
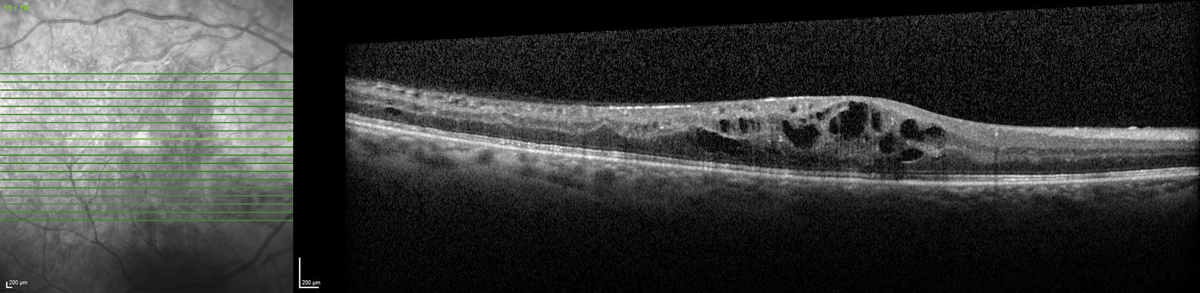
Pharmacological therapy: In DMO cases, there has been a paradigm shift in management. Laser photocoagulation is no longer recommended, and anti-VEGF intravitreal injections have emerged as first line therapy. Aflibercept and ranibizumab are listed on the PBS for management of diabetic macular oedema, and numerous clinical trials have demonstrated safety and efficacy. Intravitreal corticosteroids have maintained a role in management of chronically persistent DMO.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

