
American College of Radiologists (ACR) guidelines for the management of ‘incidentalomas’ (i.e. incidentally discovered abnormal imaging on radiology) form the basis for this discussion. ‘Incidentalomas’ appear on up to 50% of CT, MRI or PET scans, depending on the body area scanned.
The majority of time these findings are benign. For the radiologist, preparing his/her report, there may be a risk of cancer and the risk depends upon the organ in question and patient factors (perhaps unknown by the radiologist).
There are no “standards of care” to manage incidentalomas as patient care varies depending on the individual circumstances, the clinical environment, available resources, and the judgement of the practitioner.
However, the first goal is for radiologists and referring clinicians to communicate using the same standardised terminology. Agreed algorithms or flow charts can help guide management.
Important points are highlighted by two case studies:
Case Report 1: Liver lesion on CTCA for atypical chest pain.
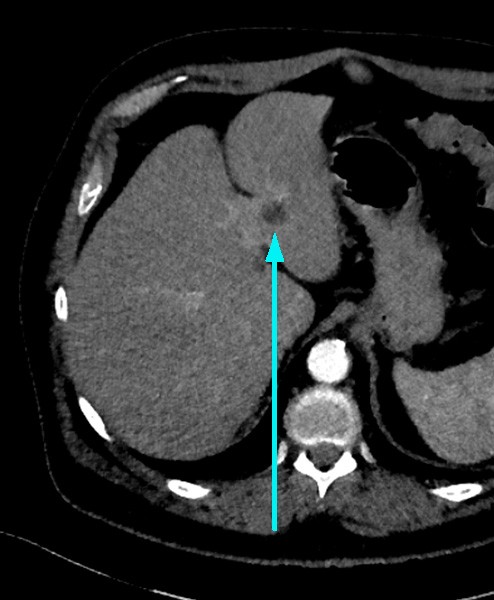
Mrs Jones, 62 years and usually very well, attends her GP feeling a right sided chest pain extending to her jaw. In addition to a thorough clinical assessment, ECG, FBC, U+E, TFT, LFT, D-dimer and troponin enzymes (all normal range), she was referred for calcium score and CT coronary angiography (CTCA) to “rule out IHD”. The CTCA images also showed a low attenuation liver lesion (below).
The report described the lesion – 14 mm well defined low attenuation lesion in the left lobe of the liver with a density of 3HU and no further investigation is required. The radiologist had used the flow chart shown here to guide the management of this finding (Fig. 1).
Case Report 2: Pancreatic cyst on a CT-IVP for haematuria.
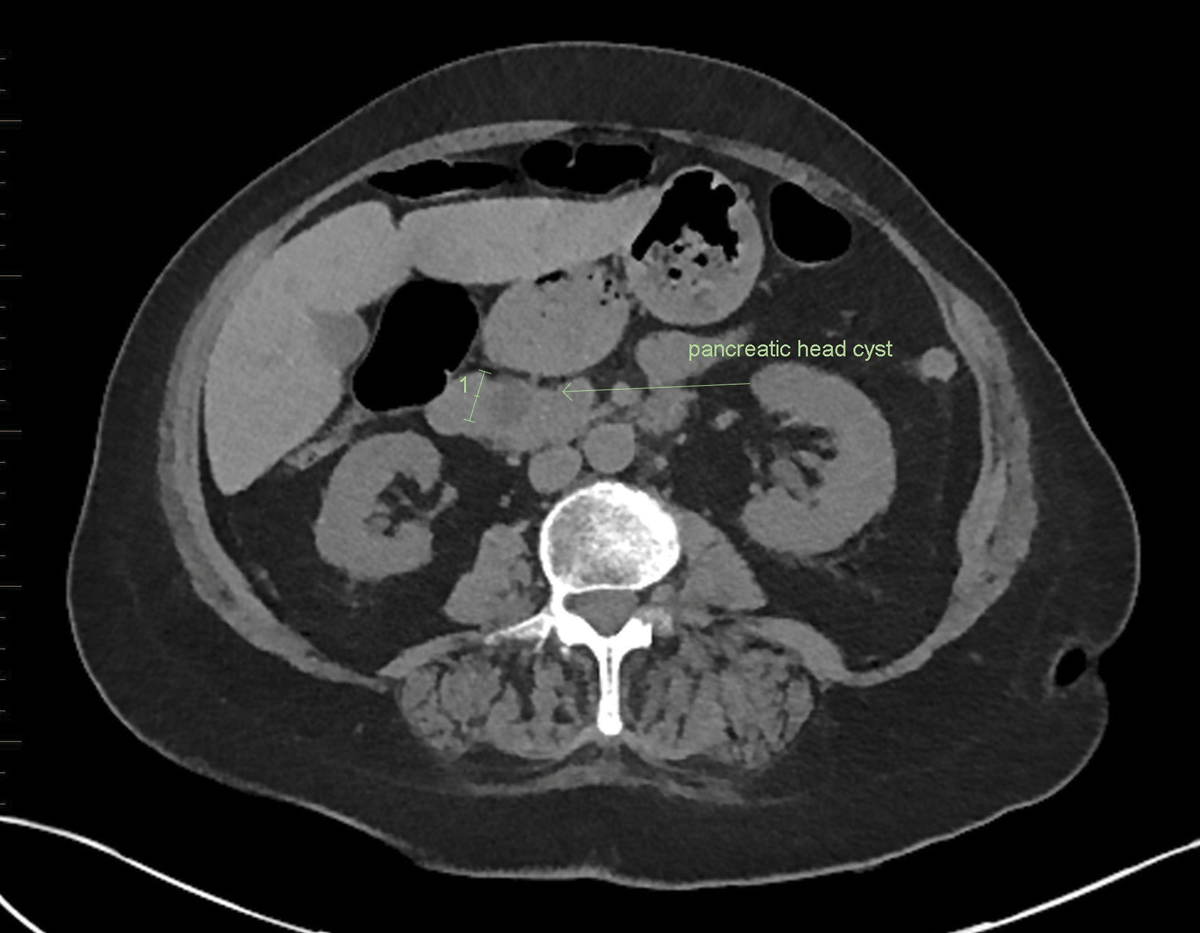
A 55 year old man presents to his GP with painless microscopic haematuria. He is referred for a CT-IVP examination to help exclude CA. The CT report describes normal renal tract appearances with no cause for haematuria identified. However, there is a 17 mm cystic lesion within the pancreas head. The lesion is not well demonstrated as the examination protocol was renal tract rather than high resolution pancreas CT protocol (equivalent of dedicated MRI pancreas protocol). The radiologist reviewed the literature for guidance and proposed on the report that the GP repeat CT (or MRI) each 6 months for 4 years, then annually for 2 years, and then in 2 years as per the chart recommendations.
The radiologist was sure to describe the absence of any “worrisome features” in relation to this cyst, to prevent further specialist review and EUS/FNA prior to surgical consideration. The patient was followed up for 9 years and although there was slight growth (<1mm per annum) the cyst remained below 25 mm and therefore no intervention was undertaken.
There has been development of 4 flow charts by the American College of Radiologists as guidance for management of these pancreatic cysts. There is a consensus that pancreatic cysts ought to be considered mucinous unless proven otherwise, certain cysts will have criteria indicating need for EUS/FNA, otherwise follow-up should be for 9-10 years in most patients, and management is modified if >80 years. Decision making should be shared by physician and patient for management of incidental pancreatic cysts (present in about 20% of abdominal MRI examinations).
Key Messages:
- Radiologists have a duty of care to identify, describe and interpret all abnormalities irrespective of their importance. Flow charts are available that depict management algorithms, and protocols cover most situations.
- Radiologists will be exposed to medicolegal risk for not reporting ‘incidentalomas’ (as happens in about 0.25% of cases); however, there is also a chance of unnecessary investigations in patients who are at low risk.
- Clinicians will need to “correlate with clinical details” when it comes to interpreting the significance of the abnormality.
- Patient and clinician agreement is essential for ongoing management of these findings, which will likely become more prevalent in the future.
Further Reading: www.acr.org/Clinical-Resources/Incidental-Findings
Author competing interests; nil relevant. Questions: Contact the editor.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

