 ED: Does the new NIPT replace the 12-week ultrasound scan?” The answer is ‘no’. We ask pathologist Dr Narelle Hadlow and obstetric radiologist Dr Anjana Thottungal to explain why – to read Anjana’s views click here: https://mforum.com.au/the-12-weeks-obstetrical-scan/ . Here is Narelle’s views.
ED: Does the new NIPT replace the 12-week ultrasound scan?” The answer is ‘no’. We ask pathologist Dr Narelle Hadlow and obstetric radiologist Dr Anjana Thottungal to explain why – to read Anjana’s views click here: https://mforum.com.au/the-12-weeks-obstetrical-scan/ . Here is Narelle’s views.

No single prenatal test can address all of the possible congenital disorders. A low risk NIPT or normal ultrasound does not guarantee a healthy baby. Good reproductive care requires an informed mother (or couple) and an informed doctor. Between them, they can consider the various screening and diagnostic tests and choose that which best meets their requirements. Therein lies good medical practice.
The whole process of reproduction is fraught. A cell must shed half of its genetic code, fuse with a half-charged cell from another person, and then build a new individual from scratch. It is hardly surprising that a variety of things can and do go wrong. Expecting that one type of test will detect all the different congenital disorders that can occur is not realistic.
How common are congenital disorders?
It is not a simple matter to estimate the frequency: recognised recessive disorders vary between ethnic groups; the advanced age of mothers (which affects the prevalence of some congenital disorders), varies across cultures, places and times. With improvements in the resolution and accessibility of ultrasound, estimates of the incidence of structural malformations are changing. And improved understanding of genetics is re-classifying many such malformations as being due to recessive or new dominant mutations. So it is a brave author who declares the frequency and diversity of congenital disorders in a population.
What types of abnormalities contribute to the congenital disorders detected at birth?
In 2006, the March of Dimes Birth Defects Foundation in the US reported on the frequency and types of congenital disorders in different countries worldwide1. Their numbers have limitations (noted above) but they provide a useful starting point.
The authors estimated that the frequency of congenital disorders in Australia was about 4%, that is, 1 in 25 babies had a congenital disorder. The impact of antenatal screening availability, principally maternal serum biochemistry and ultrasound, was not included but if it were, the frequency of congenital disorders would be approximately 5% (a number that includes both major disorders such as trisomy 13 and less serious disorders such as cleft lip.)
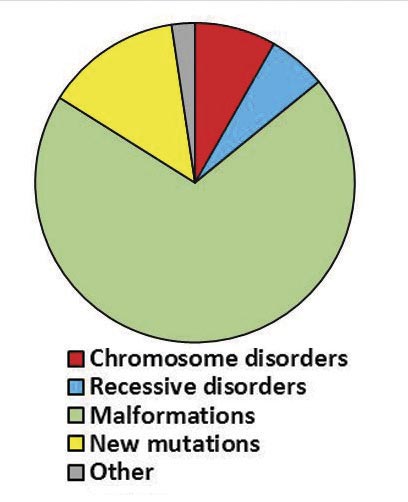
The pie-chart shows the underlying causes of those congenital disorders as understood at that time. Viewed through 2018 glasses, the proportions would be different because we now recognise that some malformations are better characterised as recessive or new dominant single gene disorders.
 Nonetheless, there are some important observations.
Nonetheless, there are some important observations.
- Only about 10% of the congenital disorders are due to abnormalities of chromosome number or structure (shown in red). For the doctor, the options for screening and investigation of possible chromosome disorders include combined first trimester screening, non-invasive prenatal testing (NIPT), amniocentesis and cytogenetic studies for couples with recurrent miscarriages. Many of these chromosome disorders lie at the severe end of the spectrum.
Remember please, NIPT is still a screening test (albeit with high sensitivity and specificity), and that confirmatory diagnostic testing of abnormal results by cytogenetics is still needed. Clinicians must also provide thorough pre-test information to patients, ensure patients are able to provide informed consent for this test and provide appropriate post-test counselling. Specific ethical issues such as sex determination should be carefully considered and a decision made with the patient as to the appropriate approach.
- Approximately 7% of the congenital disorders are autosomal and X-linked recessive (shown in blue), with the parents being unaffected carriers. It is now possible to identify couples at risk of having an affected child by reproductive carrier screening.
- The great majority of congenital disorders are structural malformations (shown in green). These range from devastating to trivial abnormalities with the more significant structural abnormalities perhaps detected on ultrasound. Some are now recognised as a feature of a specific chromosome or single-gene disorder, perhaps detected by cytogenetic and genetic testing; others will reflect a complex mix of genes, environmental factors, and chance and will only be identified by ultrasound examination.
Reference
- Christianson, A., Howson, C. & Modell, B. March of Dimes: Global Report on Birth Defects. (2006).
ED. Dr Hadlow would like to acknowledge the close assistance of Prof Graeme Suthers (Clinical Geneticist, Sonic Clinical Genetics) in preparing this article.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

