Nocturia – the complaint of waking one or more times to void – is highly prevalent in both men and women, with almost 60% over the age of 60yrs affected. It is important not to assume it is purely a urological problem and a more holistic approach to its diagnosis and management is crucial.

The greater picture
Nocturia impacts on a patient’s quality of life, and is associated with increased morbidity such as obesity, heart disease, hypertension, diabetes, depression and in the elderly, increased falls and hip fractures.
From the urologist’s standpoint, nocturia may be a symptom of benign prostatic enlargement or its consequences (either reduced functional bladder capacity from bladder overactivity or incomplete emptying from obstruction).
However, this is not always the case.
Causes are more often multifactorial and can include behavioural factors (amount, type and timing of fluid intake), sleep disturbance (insomnia, mental illness, chronic pain), obstructive sleep apnoea, underlying systemic disorder (congestive cardiac failure, poorly controlled diabetes), and drugs (e.g. lithium-induced diabetes insipidus).
How to differentiate
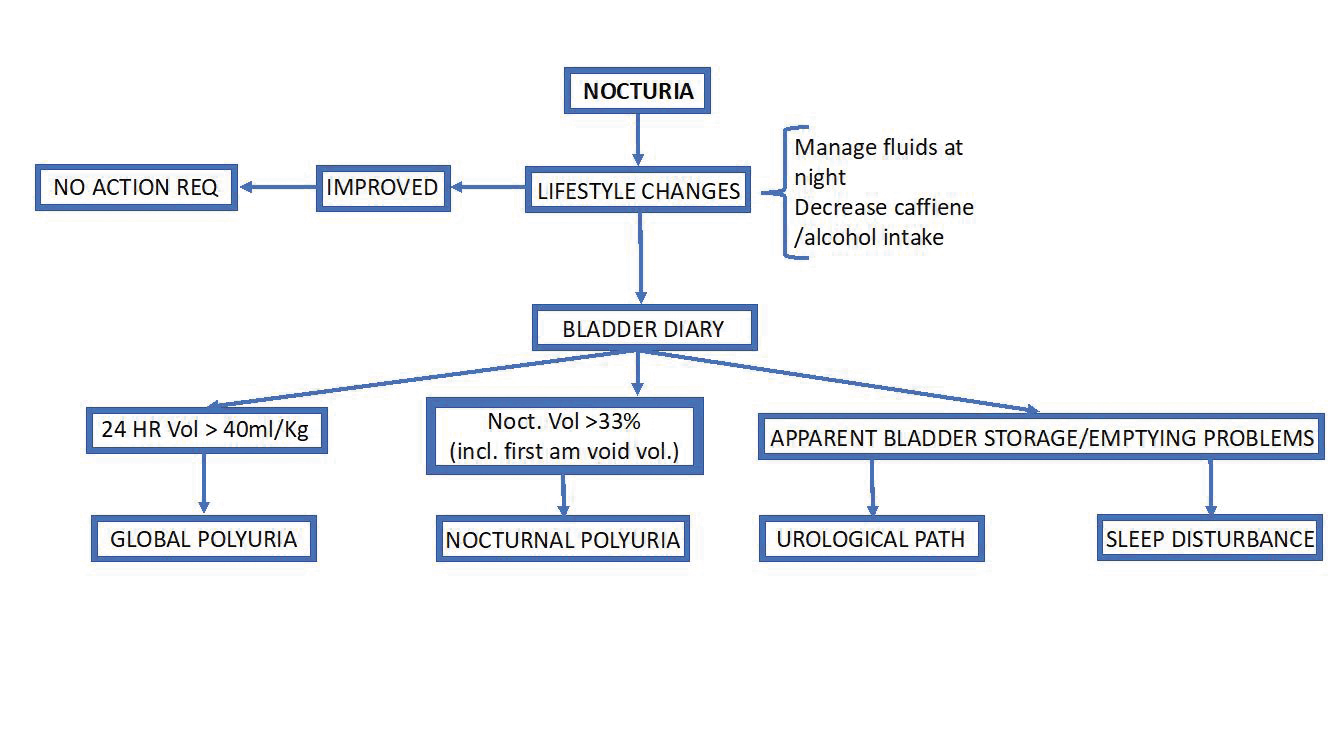
To differentiate whether nocturia is part of the symptom complex of benign prostatic enlargement or secondary to other non-urological courses, use a simple algorithm (see Figure 1).
Firstly, are lower urinary tract symptoms (LUTS) present or not – obstructive symptoms such as hesitancy, slow flow, and feeling of incomplete emptying or irritative symptoms such as frequency, urgency and urge leakage.
Only nocturia without associated LUT symptoms requires considering the possibility of non-urological causes. A detailed history that includes voiding behaviour, medical and neurological abnormalities and other reasons for sleep disturbance (i.e. waking not due to bladder sensation) will help. General examination pays specific attention to peripheral oedema.
What to recommend
Where there is no obvious pathological cause it is reasonable to recommend lifestyle changes such as reducing fluid (particularly caffeine and alcohol) intake in the evening.
At review, if these simple measures don’t work then further evaluation is required.
- A 48-72 hour bladder diary is essential, measuring input and output (see Figure 2).
- Document bladder emptying with a post-void renal US, looking for raised (>100 mls) residual urine (and remembering an over-full bladder always gives a spurious result).
- Urinalysis – to exclude microscopic haematuria that indicates other intra-vesical pathology (e.g. bladder cancer).
Medical or urological?
Look at the three-day bladder diary.
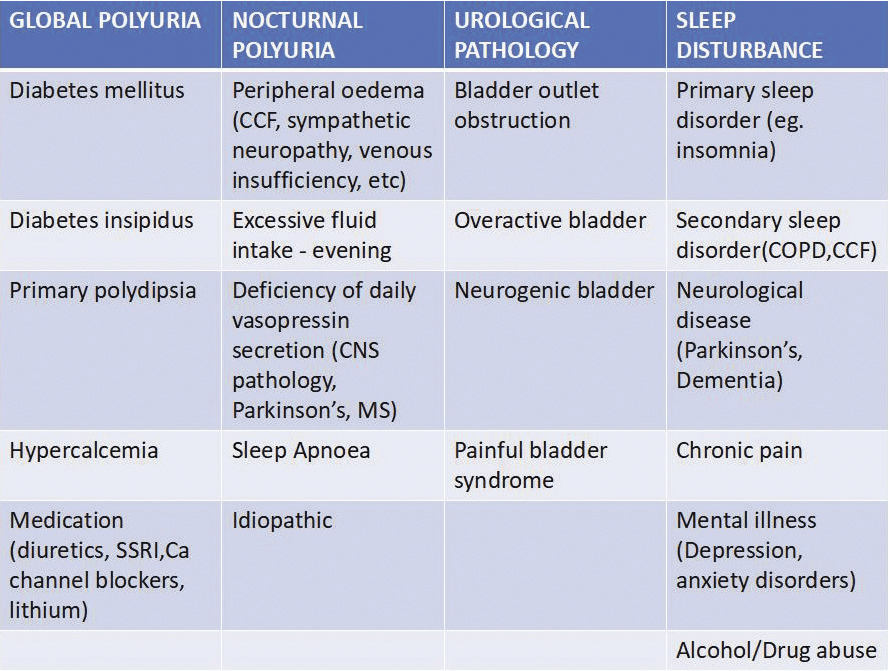
- If 24 hour urine volume > 40 ml/kg – consider polyuria and its causes. (Fig 3)
- Nocturnal urine volume (NUV) – this includes the first void of the morning, which if >33% of 24 hour volume (or > 20% in the young patient), consider nocturnal polyuria and its causes. (Fig 3)
- Individual voiding volumes can hint at diminished global and/or nocturnal bladder capacity, indicating either sleep disturbance, anxiety disorders, learned voiding dysfunction and urological disease.
Remember the cause may be multifactorial and treatment tailored for each patient may well be multimodal.
Treatment is aimed at the underlying causes and is beyond the scope of this article, however, let’s look at idiopathic nocturnal polyuria.
Idiopathic nocturnal polyuria
If it doesn’t respond to simple measures it can be managed with desmopressin, a synthetic analogue of the human hormone vasopressin (syn. antidiuretic hormone), produced by the posterior pituitary gland. Its antidiuretic activity is through vasopressin V2 receptors, influencing water reabsorption in renal tubules.
NocdurnaTM which contains desmopressin is approved for idiopathic nocturnal polyuria in the adult. Taken an hour before bedtime as a wafer, there are gender-specific recommendations of 25 mcgm a day for women and 50 mcgm a day for men.
The most commonly reported side effects of desmopressin include headaches, dry mouth, nausea, oedema and hyponatraemia (which is due to fluid overload and most significant in those >65 years age; sodium level is measured before starting the drug and 4-8 days after starting and 1 month later; regular monitoring after this is recommended).
Fig 3.
References available on request
Author competing interests declaration: nil relevant. Questions? Contact the editor.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.