Chronic kidney disease (CKD) affects one in ten adult Australians (AIHW figures; a probable underestimate of prevalence). Strategies have been used to help identify CKD in the community.

These include automatic serum creatinine-based estimated glomerular filtration rate (eGFR) reporting by laboratories, promotion of kidney health checks (blood pressure, eGFR, albuminuria), CKD management guidelines for GPs, apps providing guidance to primary healthcare providers and patients and web-based clinical risk prediction tools for CKD.
There are pitfalls in relying solely on eGFR to detect CKD. These include biological variations in serum creatinine, potential laboratory analytical error and external factors that can influence accurate serum creatinine. In fact, the widespread use of eGFR to identify CKD has led to the misclassification and over-diagnosis of people without true CKD, resulting in anxiety and unnecessary investigations.
Even though physiological reduction (i.e. age-related sclerosis) in eGFR occurs with increasing age, it is important to distinguish from other kidney pathology i.e. that needing appropriate referral and targeted investigations. Irrespective of the aetiology, reduced eGFR below 60ml/min/1.73m2 is associated with a heightened risk of mortality and many other diseases, including cardiovascular disease (CVD) and cancer.
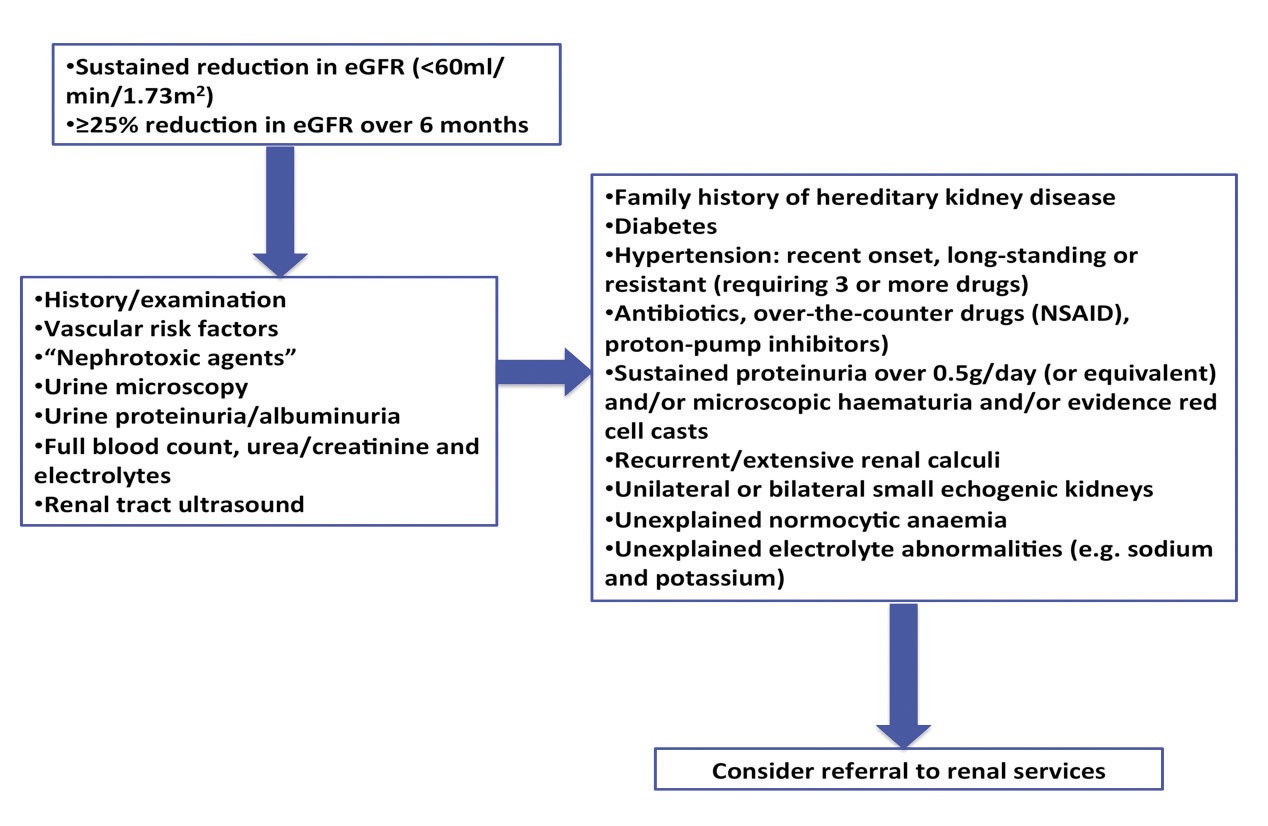
A major challenge is differentiating a “benign” process from the more serious. The flow diagram shows a simple diagnostic pathway to assist in the decision-making process.
In patients with established moderate to severe CKD (i.e. eGFR <60ml/min /1.73m2), a shared-care model between general practitioners, nephrologists and other specialists is essential. Target CVD risk factors and proteinuria, to (hopefully) delay the progression of CKD and reduce future CVD events.
Some practical evidence-based management tips are:
- Diabetic and non-diabetic CKD with urine albumin excretion of <30 mg/mmol, target blood pressure to ≤140/90mmHg.
- Diabetic or non-diabetic CKD with urine albumin excretion >300 mg/mmol: use angiotensin-converting enzyme inhibitor (ACE-I) or angiotensin receptor blocker (ARB). Aim to reduce urine albumin excretion of <100 mg/mmol and target blood pressure to ≤130/80mmHg. Monitor eGFR and serum potassium.
- In CKD patients with diabetes, target glycated haemoglobin to 7.0% (unless risk of hypoglycaemia).
- Maintain serum bicarbonate within normal range with oral bicarbonate supplementation.
- Dietary information and advice regarding the restriction of salt and intake of protein, potassium and phosphate according to CKD severity.
- Appropriate dose reduction of medications that are excreted by the kidneys.
- Ensure patients seek appropriate advice about prescribed nephrotoxic agents, over the counter medications or protein supplements.
- CKD patients should be considered high risk for developing CVD. Manage using general population treatment guidelines.
- Timely referral to specialist renal services (as per flowchart).
 References available on request.
References available on request.
Author competing interests: nil relevant. Questions? Contact the editor.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

