As part of a contemporary multimodal approach, spinal pain management procedures (SPMPs) are usually not a permanent ‘pain cure’ (analgesia lasts weeks-to-months) but in selected patients, they provide a ‘therapeutic window’ of pain relief to facilitate physical and psychological rehabilitation, reduced pain neuro-sensitisation (wind-up) and decreased analgesic use (particularly opioids).

Adverse outcomes of SPMPs include lack of efficacy (particularly in patients exposed to psychosocial stressors), worsening pain, tissue damage, neuro-trauma, infection, bleeding, drug reactions, radiation exposure and, rarely, paralysis or death.
About 20-40% of chronic neck and low back pain (LBP) is associated with facet joint arthropathy; 20% of LBP is due to sacroiliac joint arthropathy or cluneal nerve entrapment over the iliac crest and 10% of leg or arm pain is ‘radicular’ due to a spinal nerve root lesion (e.g. disc protrusion).
The most commonly performed SPMPs are: facet joint steroid injection (FJI), medial branch (nerves innervating facet joints) radiofrequency treatments (RF), transforaminal epidural steroid injection (TFESI), sacroiliac joint steroid injection (SIJI) and cluneal nerve block (CNB). RF treatments include pulsed RF (temporary electromagnetic inhibition of nerve function) and thermal RF neurotomy (nerve ‘cautery’ at 90°C).
Evidence for effective analgesia with FJI and RF in the spinal pain population is limited. However, there are individual responders. It is reasonable to consider FJI or RF in patients with chronic spinal pain who are over 60 years of age, or for neck pain following whiplash.
FJI or RF should be ordered based on clinical presentation (table 1); spinal imaging is not routinely required. If an initial FJI is ineffective (<50% pain reduction) reconsider the need for further injections. If FJI is effective but lasts <3M, then RF may prolong the analgesic effect. For unilateral buttock and thigh pain, consider a CNB (treats entrapment of cluneal nerves over the iliac crest), or a SIJI.
 TFESI is only indicated for subacute (<6M) radicular leg pain where multimodal treatment is ineffective or there is significant disability. A spinal MRI or CT scan is required prior to injection to confirm a targetable nerve root lesion. Do not order a cervical TFESI for radicular arm pain without specialist advice. These blocks are poorly-effective and associated with rare but catastrophic neurovascular events such as stroke, due to inadvertent intra-arterial injection of particulate steroids.
TFESI is only indicated for subacute (<6M) radicular leg pain where multimodal treatment is ineffective or there is significant disability. A spinal MRI or CT scan is required prior to injection to confirm a targetable nerve root lesion. Do not order a cervical TFESI for radicular arm pain without specialist advice. These blocks are poorly-effective and associated with rare but catastrophic neurovascular events such as stroke, due to inadvertent intra-arterial injection of particulate steroids.
Indications and patient selection for SPMPs are listed in table 1.
References available on request. The author acknowledges the assistance of Dr Luke Wheeler.
Author competing interests; nil relevant disclosures. Questions? Contact the author at eric.visser@nd.edu.au
Table 1. Spinal Pain Management Procedures (SPMPs)
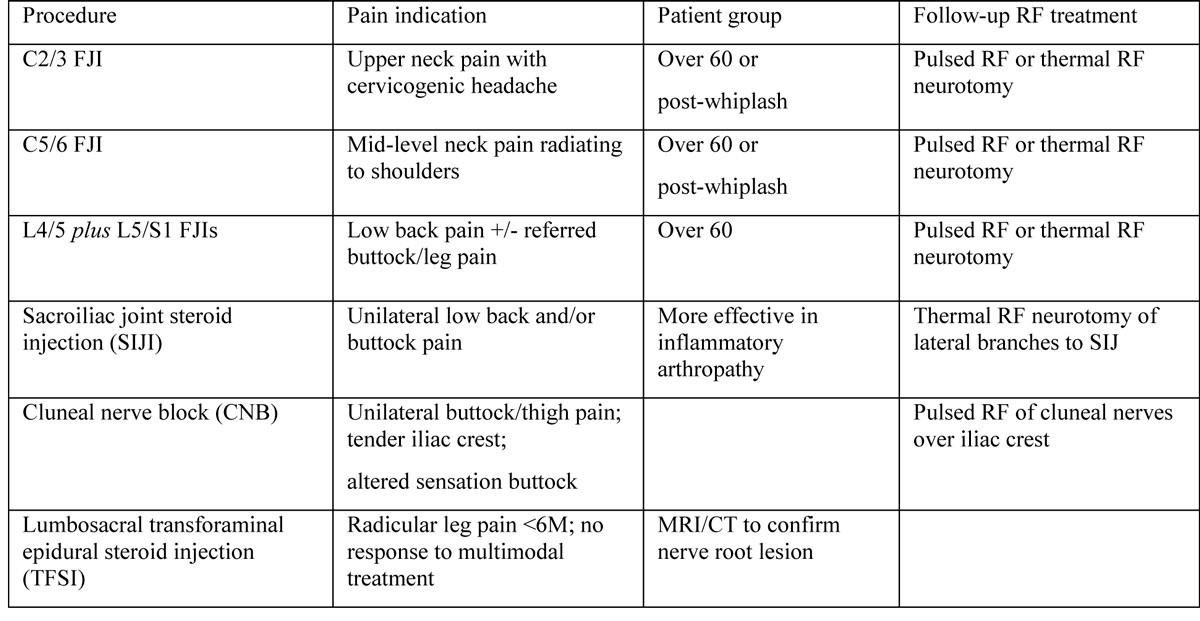 FJI=facet joint steroid injection; RF=radiofrequency treatment of medial nerve branch of spinal dorsal ramus; SIJ(I)=sacroiliac joint (injection).
FJI=facet joint steroid injection; RF=radiofrequency treatment of medial nerve branch of spinal dorsal ramus; SIJ(I)=sacroiliac joint (injection).
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

